OneEyedDiva
SF VIP
- Location
- New Jersey
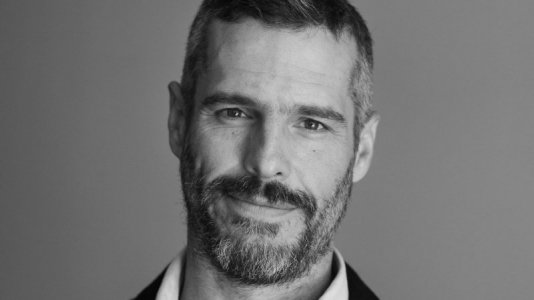
Dr. B.J. Miller treats patients in need of palliative and hospice care. Even though my husband was already in the ICU, I experienced (along with my one of my stepdaughters),having to choose which kind of care he should receive because my husband was no longer able to do it himself. He died two weeks later. Highlights from the article:
To the caregivers: Don't be afraid to leave the room
Patients may have deathbed delirium causing behavior to range from sweet to insufferable"
Read more here:
https://www.cnn.com/2019/07/18/opinions/doctor-advice-facing-death-miller/index.html
I sure wouldn't mind it if Dr. Miller was one of the last people I saw when I'm dying.
"
"Don’t wait for your doctor to bring up hospice
You don’t need to be dying to receive palliative care
It's okay to laughTo the caregivers: Don't be afraid to leave the room
Patients may have deathbed delirium causing behavior to range from sweet to insufferable"
Read more here:
https://www.cnn.com/2019/07/18/opinions/doctor-advice-facing-death-miller/index.html
I sure wouldn't mind it if Dr. Miller was one of the last people I saw when I'm dying.
"
Last edited:


